Rice bioengineers 3D-print implants to seed multiple layers of tissue
Who ever said bioengineers can’t get their groove on?

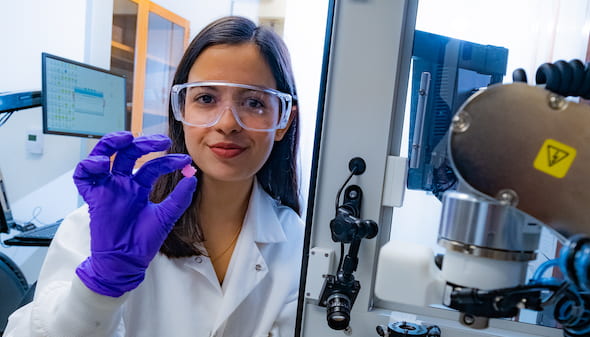
Rice research scientist Maryam Elizondo holds a 3D-printed scaffold engraved with grooves for the deposition of live cells for implantation. The scaffold facilitates the growth of new tissues as it degrades. By protecting cells in grooves along the printed lines, Rice researchers designed the scaffold to enable different tissue-type layers within one scaffold. Photo by Jeff Fitlow
The Rice University team led by Antonios Mikos says otherwise with its development of a groovy method to seed sophisticated, 3D-printed tissue-engineering scaffolds with living cells to help heal injuries.
The researchers are literally carving grooves into plastic threads used to build the scaffolds. The grooves are then seeded with cells or other bioactive agents that encourage the growth of new tissue.
The strategy protects cells from the heat and shear stresses that would likely kill them in other scaffold fabrication processes. It also provides a way to layer cells that ultimately become different kinds of tissue, like bone and cartilage, in a mechanically stable platform.
The beauty of it is the 3D printer cuts the grooves into a thermoplastic, inserts the cells at the proper temperature and creates a three-dimensional implant, based on medical images, in a single process.
The research is the topic of a paper in Bioprinting.
Unlike cell-supporting hydrogel scaffolds under development at Rice and elsewhere, this process creates hard implants that would be surgically inserted to heal bone, cartilage or muscle, Mikos said. Like hydrogels, the biocompatible implants would degrade over time and leave only natural tissue.
“The major innovation here is our ability to spatially load a scaffold that is 3D printed with different cell populations and with different bioactive molecules,” Mikos said.
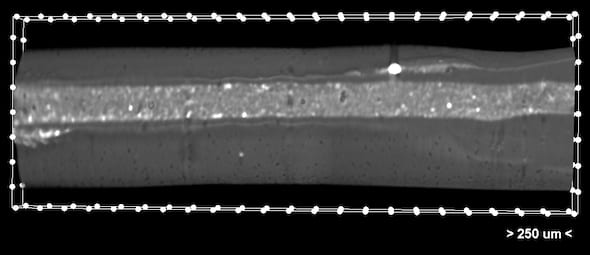
A microCT image shows a grooved thread that holds the low-viscosity bioink. They are part of a 3D-printed scaffold developed at Rice University to facilitate the growth of new tissue like bone and cartilage. The scaffolds degrade over time to leave layers of natural tissues in place. Courtesy of the Rice Biomaterials Lab
Until now, 3D-printed scaffolds were generally seeded with uniform distributions of cells, he said. “If we wanted different cell populations at different points in the scaffold, we could not do that. Now we can.”
“The fibers are cylinders that we engrave with a needle to give it a groove as it’s printing,” said Rice research scientist Maryam Elizondo, co-lead author of the paper with alumnus Luis Diaz-Gomez. Once the groove is set and cooled just enough, the printer then deposits a cell-infused ink. “We do that for every fiber for every layer of the scaffold.”
Elizondo compared the grooved threads, which are about 800 microns wide, to taco shells that keep the contents inside without spilling; here, the addition of grooves and ultraviolet-activated crosslinkers keep the cell ink inside. She said it takes about half an hour to completely print a thumbnail-sized implant.
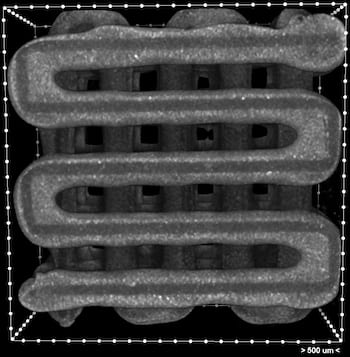
A microCT image shows a 3D-printed scaffold with clear grooves meant for the deposition of live cells. The grooved lines hold ink deposited during the printing process. Scaffolds can be made in any shape, based on medical images, to fill the site of a wound. Courtesy of the Rice Biomaterials Lab
Mikos said the scaffold isn’t limited to cells. “We can also load different growth factors on different levels,” he said. “Very high temperatures would deactivate them, but here we can deposit growth factor-loaded microparticles inside the grooves as they cool. That would preserve the bioactivity of the molecule.
“This is a great success for the Center for Engineering Complex Tissues,” he said of the multiuniversity collaborative he helped create. “That was the goal when we built the center: to develop advanced materials with unique properties that can be used for tissue engineering applications that address unmet clinical needs. And this is a perfect example.”
Co-authors of the paper are Rice graduate students Gerry Koons and Letitia Chim; postdoctoral fellow Mani Diba; Biomaterials Lab Associate Director Anthony Melchiorri; and Rice alumna Elizabeth Cosgriff-Hernandez, a professor of biomedical engineering at the University of Texas at Austin. Mikos is the Louis Calder Professor of Bioengineering and a professor of chemical and biomolecular engineering, of materials science and nanoengineering and of chemistry.
The National Institutes of Health supported the research.